Industrial safety expert conclusion and explanatory letters, Uncategorized
Industrial safety expert conclusion and explanatory letters 4
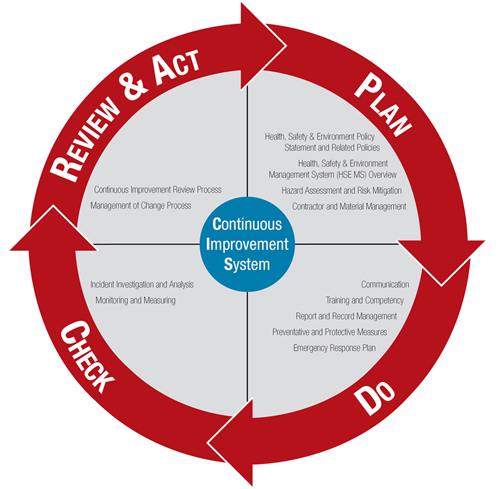
Occupational safety and health (OSH), also commonly referred to as occupational health and safety (OHS), occupational health, or occupational safety, is a multidisciplinary field concerned with the safety, health, and welfare of people at work (i.e. in an occupation). These terms also refer to the goals of this field, so their use in the sense of this article was originally an abbreviation of occupational safety and health program/department etc.
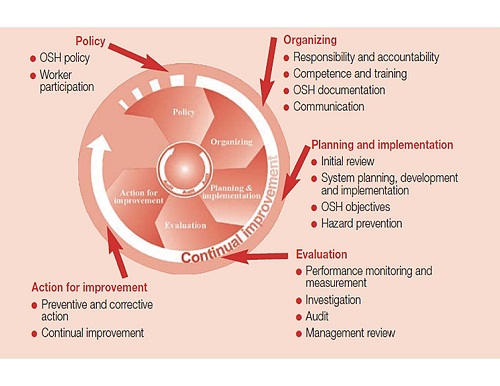
The goal of an occupational safety and health program is to foster a safe and healthy occupational environment. OSH also protects all the general public who may be affected by the occupational environment.
Globally, more than 2.78 million people die annually as a result of workplace-related accidents or diseases, corresponding to one death every fifteen seconds. There are an additional 374 million non-fatal work-related injuries annually. It is estimated that the economic burden of occupational-related injury and death is nearly four per cent of the global gross domestic product each year. The human cost of this adversity is enormous.
In common-law jurisdictions, employers have the common law duty (also called duty of care) to take reasonable care of the safety of their employees. Statute law may, in addition, impose other general duties, introduce specific duties, and create government bodies with powers to regulate occupational safety issues: details of this vary from jurisdiction to jurisdiction
Definition
As defined by the World Health Organization (WHO) “occupational health deals with all aspects of health and safety in the workplace and has a strong focus on primary prevention of hazards.” Health has been defined as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.” Occupational health is a multidisciplinary field of healthcare concerned with enabling an individual to undertake their occupation, in the way that causes least harm to their health. It aligns with the promotion of health and safety at work, which is concerned with preventing harm from hazards in the workplace.
Since 1950, the International Labour Organization (ILO) and the WHO have shared a common definition of occupational health. It was adopted by the Joint ILO/WHO Committee on Occupational Health at its first session in 1950 and revised at its twelfth session in 1995. The definition reads:
“The main focus in occupational health is on three different objectives: (i) the maintenance and promotion of workers’ health and working capacity; (ii) the improvement of working environment and work to become conducive to safety and health and (iii) development of work organizations and working cultures in a direction which supports health and safety at work and in doing so also promotes a positive social climate and smooth operation and may enhance productivity of the undertakings. The concept of working culture is intended in this context to mean a reflection of the essential value systems adopted by the undertaking concerned. Such a culture is reflected in practice in the managerial systems, personnel policy, principles for participation, training policies and quality management of the undertaking.”
— Joint ILO/WHO Committee on Occupational Health
Those in the field of occupational health come from a wide range of disciplines and professions including medicine, psychology, epidemiology, physiotherapy and rehabilitation, occupational medicine, human factors and ergonomics, and many others. Professionals advise on a broad range of occupational health matters. These include how to avoid particular pre-existing conditions causing a problem in the occupation, correct posture for the work, frequency of rest breaks, preventive action that can be undertaken, and so forth. The quality of occupational safety is characterized by (1) the indicators reflecting the level of industrial injuries, (2) the average number of days of incapacity for work per employer, (3) employees’ satisfaction with their work conditions and (4) employees’ motivation to work safely.
“Occupational health should aim at: the promotion and maintenance of the highest degree of physical, mental and social well-being of workers in all occupations; the prevention amongst workers of departures from health caused by their working conditions; the protection of workers in their employment from risks resulting from factors adverse to health; the placing and maintenance of the worker in an occupational environment adapted to his physiological and psychological capabilities; and, to summarize, the adaptation of work to man and of each man to his job.
Given the high demand in society for health and safety provisions at work based on reliable information, occupational safety and health (OSH) professionals should find their roots in evidence-based practice. A new term is “evidence-informed decision making”. A working definition of evidence-based practice could be: evidence-based practice is the use of evidence from literature, and other evidence-based sources, for advice and decisions that favor the health, safety, well-being, and work ability of workers. Therefore, evidence-based information must be integrated with professional expertise and the workers’ values. Contextual factors must be considered related to legislation, culture, financial, and technical possibilities. Ethical considerations should be heeded.
History
Harry McShane, age 16, 1908. Pulled into machinery in a factory in Cincinnati and had his arm ripped off at the shoulder and his leg broken without any compensation.
The research and regulation of occupational safety and health are a relatively recent phenomenon. As labor movements arose in response to worker concerns in the wake of the industrial revolution, worker’s health entered consideration as a labor-related issue.
In 1700, De Morbis Artificum Diatriba outlined the health hazards of chemicals, dust, metals, repetitive or violent motions, odd postures, and other disease-causative agents encountered by workers in more than fifty occupations. In the United Kingdom, the Factory Acts of the early nineteenth century (from 1802 onwards) arose out of concerns about the poor health of children working in cotton mills: the Act of 1833 created a dedicated professional Factory Inspectorate. : 41 The initial remit of the Inspectorate was to police restrictions on the working hours in the textile industry of children and young persons (introduced to prevent chronic overwork, identified as leading directly to ill-health and deformation, and indirectly to a high accident rate). However, on the urging of the Factory Inspectorate, a further Act in 1844 giving similar restrictions on working hours for women in the textile industry introduced a requirement for machinery guarding (but only in the textile industry, and only in areas that might be accessed by women or children).[13] : 85
In 1840 a Royal Commission published its findings on the state of conditions for the workers of the mining industry that documented the appallingly dangerous environment that they had to work in and the high frequency of accidents. The commission sparked public outrage which resulted in the Mines Act of 1842. The act set up an inspectorate for mines and collieries which resulted in many prosecutions and safety improvements, and by 1850, inspectors were able to enter and inspect premises at their discretion.[
Otto von Bismarck inaugurated the first social insurance legislation in 1883 and the first worker’s compensation law in 1884 – the first of their kind in the Western world. Similar acts followed in other countries, partly in response to labor unrest.

